Bpci Quality Measures

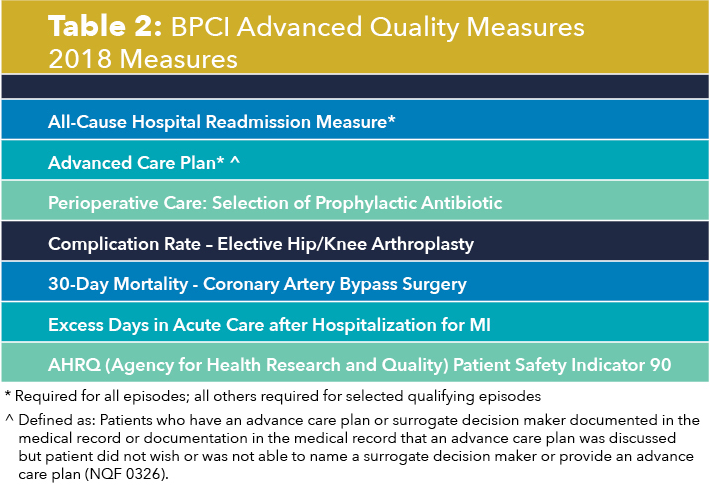
All cause hospital readmission measure national quality forum nqf 1789 advance care plan nqf 0326 specific clinical episodes.
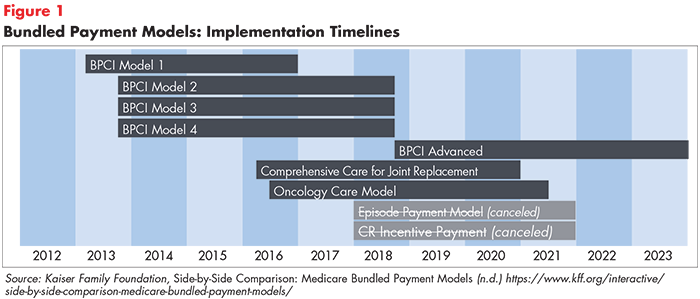
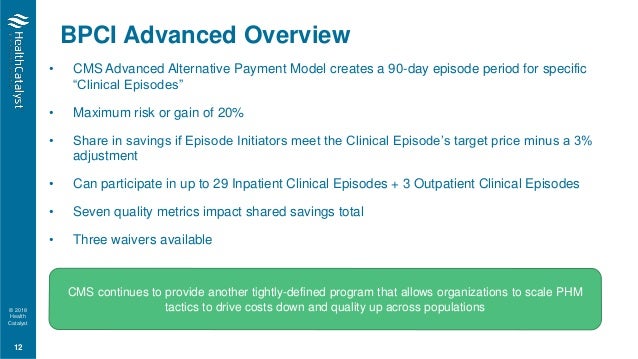
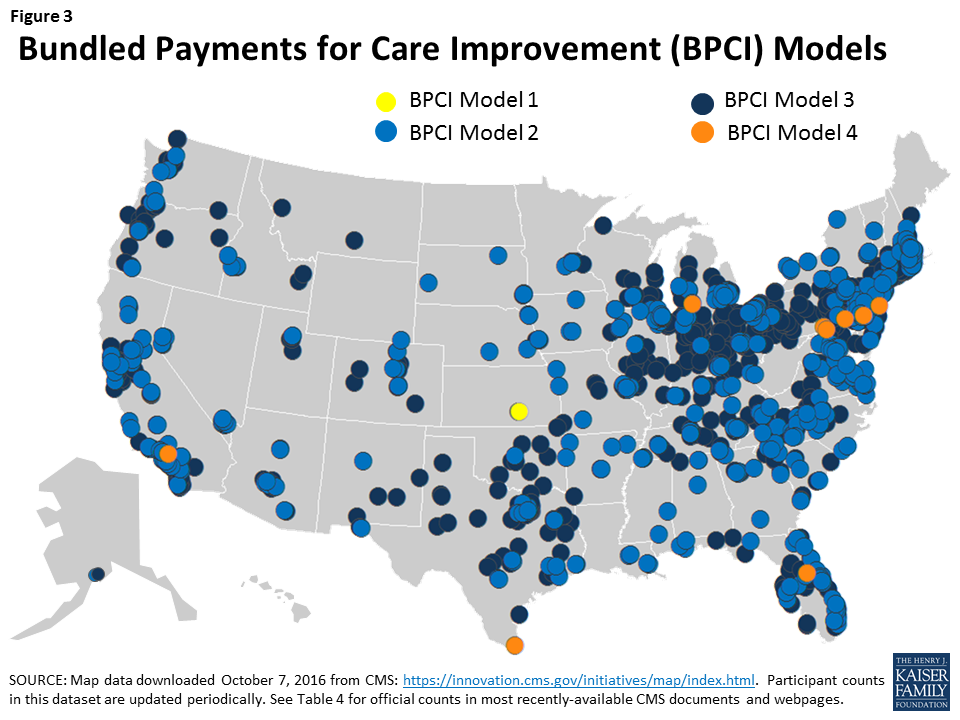
Bpci quality measures. The centers for medicare and medicaid services cms on aug. The bpci advanced version of this measure uses a one year period. The bundled payments for care improvement bpci initiative was comprised of four broadly defined models of care which linked payments for the multiple services beneficiaries received during an episode of care. Bpci advanced qualifies as an advanced alternative payment model advanced apm under the quality payment program.
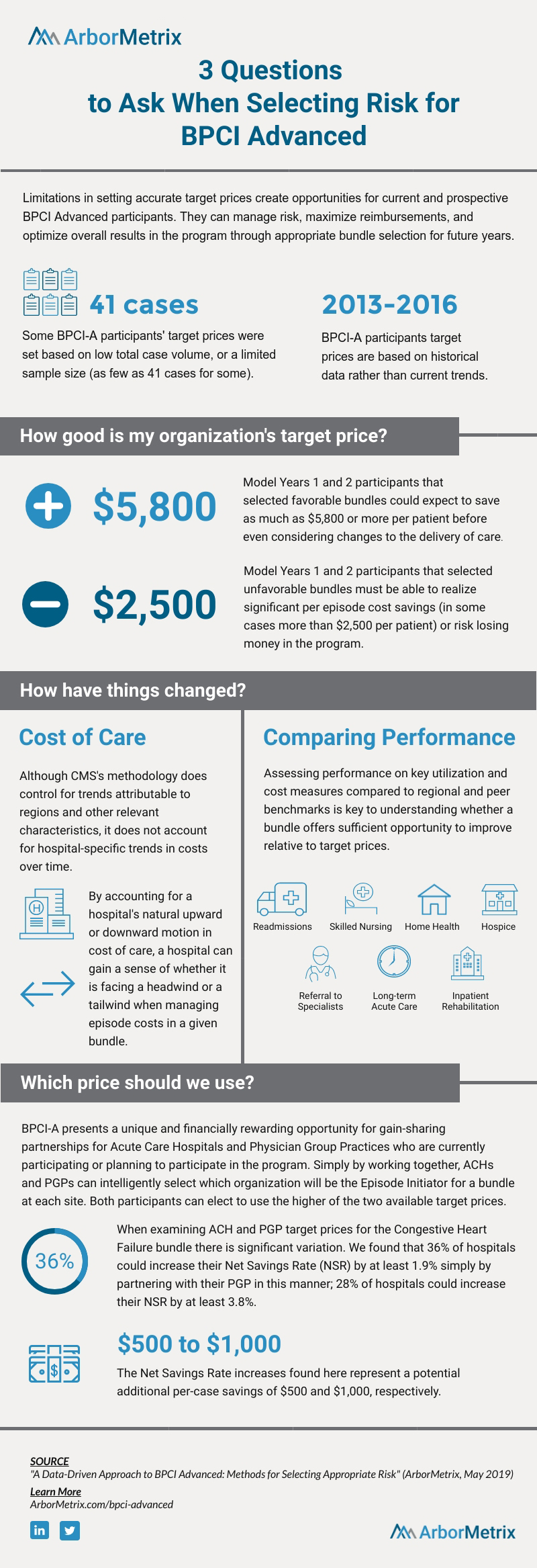
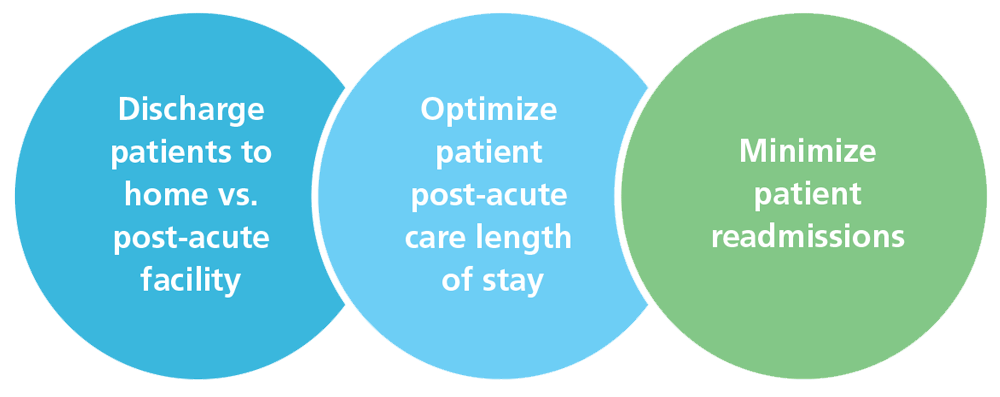
Key milestones and dates bpci advanced builds upon lessons gleaned from current and previous cms models demonstrations and programs. Advanced voluntary bundled payment model. Quality measures background the bundled payments for care improvement bpci advanced model reimburses participants for clinically appropriate services provided to medicare beneficiaries throughout an entire clinical episode using a voluntary bundled payment methodology. The cqs adjustment will not adjust the positive total.
The hospital level rscr following elective primary tha and or tka measure is one component of the bpci advanced composite quality score cqs calculation. The required quality measure list for bpci advanced includes both process and outcome quality measures. Composite quality score the hospital wide all cause unplanned readmission measure is one component of the bpci advanced composite quality score cqs calculation. The centers for medicare and medicaid services cms on july 3 released the quality measure sets for bundled payments for care improvement bpci advanced model year 3 which qualifies as an advanced alternative payment model under the quality payment program.
Composite quality score the acp measure is one component of the bpci advanced composite quality score cqs calculation. Quality measures the cms innovation center s bpci advanced model rewards health care providers for delivering services more efficiently supports enhanced care coordination and recognizes high quality care. The cms innovation center uses the cqs to adjust a portion of any positive total reconciliation amount and any negative total reconciliation amount. The cms innovation center uses the cqs to adjust a portion of any positive total reconciliation amount and any negative total reconciliation amount.
Bpci advanced qualifies as an advanced alternative payment model under the quality payment program.